Alarm Committee Wins National Award
by Jennifer L.W. Fink
 Long before anyone had heard the term “alarm fatigue,” Maria Cvach, MSN, RN, CCRN, was studying the problem of incessant alarms at The Johns Hopkins Hospital. So many alarms were going off that it was difficult for nurses to know which alarms truly required attention and which represented a simple glitch—and Cvach and others worried that important alarms might get missed.
Long before anyone had heard the term “alarm fatigue,” Maria Cvach, MSN, RN, CCRN, was studying the problem of incessant alarms at The Johns Hopkins Hospital. So many alarms were going off that it was difficult for nurses to know which alarms truly required attention and which represented a simple glitch—and Cvach and others worried that important alarms might get missed.
That concern blossomed into a multi-disciplinary Alarm Committee that has spent the past six years working to improve patient safety by tweaking alarm settings to provide meaningful information to nurses on a need-to-know basis. Their innovative work has not only created quieter units; according to the ECRI Institute, it’s created a blueprint that other hospitals can use to improve patient safety.
The Institute awarded their 2012 ECRI Health Devices Achievement Award to the JHH Alarm Committee for developing alarm improvements that are easy for other hospitals to implement. Cvach, currently a DNP student at the Johns Hopkins Univer-sity School of Nursing, says that “it’s relatively simple to safely tweak alarm settings, rather than just guessing. It’s just a matter of getting data and using them to change practice.”
Cvach and her team relied heavily on data while designing alarm reduction programs. “It took us two years to figure out how to sort and categorize the types of alarms,” she says. “Then we ran a one-year pilot study with four different interventions and studied the effect of that. When we learned what worked, we started bringing in the rest of the hospital.”
The Alarm Committee quickly realized that tweaking the default settings on physiologic alarms would result in fewer, but actionable, alarms. They also realized that each hospital unit had its own unique needs and challenges, so individual units were allowed to make decisions about what kinds of changes to institute.
The PICU, for instance, deals with patients from birth to age 21. “So we customized our defaults based on age ranges,” says Judy Ascenzi, MSN, RN. Nurses still further tweak the settings based on their patients’ conditions, but starting with age-appropriate settings helps save time.
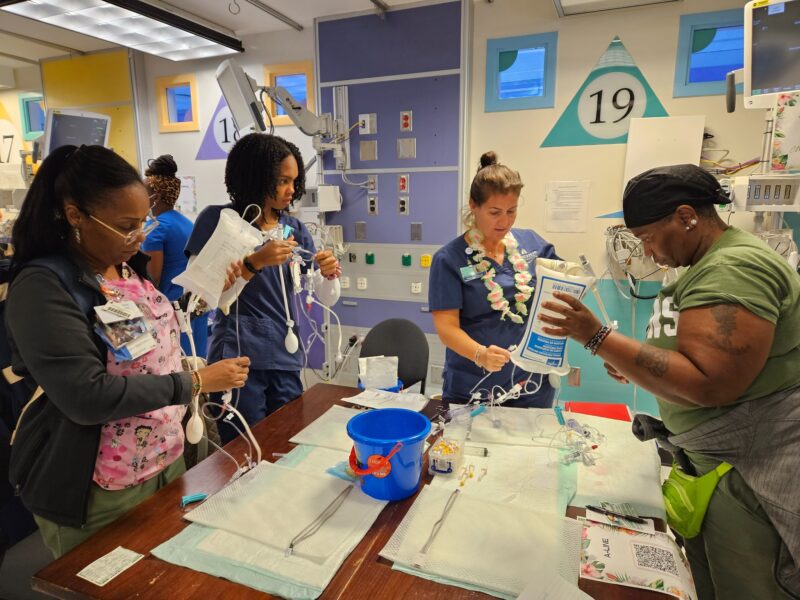
The PICU also divided their unit into zones. “Our geographical footprint is huge, so it would make no sense for the nurse for bed 1 to get alarms about the patient in bed 41,” Ascenzi says. “Instead, we assign nurses to a care zone. The monitor in that zone only shows alarms for patients in that zone.”
As a result, the PICU today is a quieter place than it once was. Nurses can concentrate on their work, confident that they’ll receive important alarms. Patients and families can rest, confident that nurses will come when needed.
And that, after all, is the goal of the Alarm Committee.
“Families lose trust in staff when they don’t come and check alarms, and noise is a huge factor in terms of healing,” Cvach says. “Less noise is better for the patient and better for the family.”